|
|||||||
Fracture Management for the Primary Care Physician
The primary care physician who wishes to manage fractures needs to know what is "safe" to treat, and what should be referred to a specialist.
There are some fractures that should be referred to a specialist. These include:
- Fractures around or involving joint surfaces. Even slight displacement involving the joint surface can lead to disabling long-term problems like degenerative arthritis and pain.
- Fractures with significant displacement or angulation on X-rays, or with obvious deformity on clinical exam. The degree of displacement or angulation that can be accepted depends on the particular bone involved, and the age of the patient. However, 50% displacement and 30 degree angulation is the upper limit of acceptability for most bones. Depending on your experience, and for the sake of safety, you may pick 15 degrees of angulation or less as your upper limit.
- Skin compromise in terms of extensive or deep abrasion or laceration associated with the fracture may preferably be treated by a specialist. This is especially important if there is some concern if it is an open fracture.
- Neurovascular concerns are best referred to a specialist. Any significant swelling, severe pain distal to the fracture and muscle weakness are warning signs.
- Epiphyseal plate injuries, except for certain Type I epiphyseal plate injuries listed below are best referred out. There is no need for you to be responsible for long-term growth problems.
- Fractures of certain specific regions are safer treated by a specialist because of their tendency to cause problems - spine, hip, femur, tibia, calcaneus, talus, elbow and forearm.
The following are examples of "safe" fractures that can usually be treated by the primary care physician. However, it is important for any physician who wishes to venture into fracture treatment to understand that there are pitfalls even in "safe areas", and vigilance is ever required.
 |
Fracture Clavicle
Treatment: Clavicular splint for 6 weeks in children, and 8 to 10 weeks in adults |

|
|
Fracture neck of Humerus
Treatment: Arm sling or shoulder immobilizer for 6 weeks in children, and 8 to 10 weeks in adults |

|
|
|
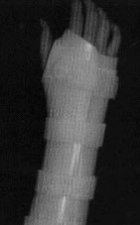
Fractures of lower radius and ulna
Treatment: Casting or Wrist Fracture Brace for 4 to 6 weeks in children, and 6 to 8 weeks in adults |
|
|
|
Fracture of metacarpal
Treatment: Wrist-Hand-Finger Orthosis (WHFO) immobilizing the MP and IP joints for 4 to 6 weeks. |
|
|
|
Fracture phalanx (finger)
Treatment: Wrist-Hand-Finger Orthosis (WHFO) for proximal phalanx; Finger aluminum splint for middle and distal phalanx, immobilizing the joint proximal and distal to the fracture for about 3 weeks. |
|
Fracture metatarsal
Treatment: Regular walking cast, or a removeable walking cast (Pediwalker) for 6 to 8 weeks |
|
|
|
Fracture Toe
Treatment: Buddy taping for 3 weeks, using sticky tape or Coflex bandage. |
Contusion or Type I Epiphyseal plate injuries in children
Difficult to distinguish when there is no displacement. If there is exquisite tenderness at the epiphyseal plate, the diagnosis is assumed.
- Swelling expected, but skin is not compromised
- Neurovascular exam is normal
- X-rays may be normal or may show slight widening of the epiphyseal plate
Treatment: Immobilisation of the joint involved, e.g.,
- Type I Epiphyseal plate injury of lower fibula - short leg walking cast or Pediwalker for 3 weeks
- Type I Epiphyseal plate injury of lower radius/ulna - short arm cast or Wrist fracture brace for 3 weeks
-
Type I Epiphyseal plate injury of base of 1st Metacarpal - thumb spica cast or thumb spica fracture brace
NOTICE: The information presented is for your information only, and not a substitute for the medical advice of a qualified physician. Neither the author nor the publisher will be responsible for any harm or injury resulting from interpretations of the materials in this article.
Questions
or comments? Post your thoughts in the Orthoseek
Message Forum!
Find a pediatric orthopedic surgeon
in an area near you.
Home | About Us | Orthopaedic Topics | Message Forum
![]()
Comments, questions, or suggestions are welcome. Please
contact us using this form.